Wide Complex Monomorphic Ventricular Tachycardia
Many wide complex tachycardias originate in the ventricles, but some do not.
The ones that do not may include:
- Aberrant SVT, like a bundle branch block
- Ventricular reentry problem where the ventricles contract too early after partial repolarization (like a pre-excited tachycardia or Wolff-Parkinson White syndrome)
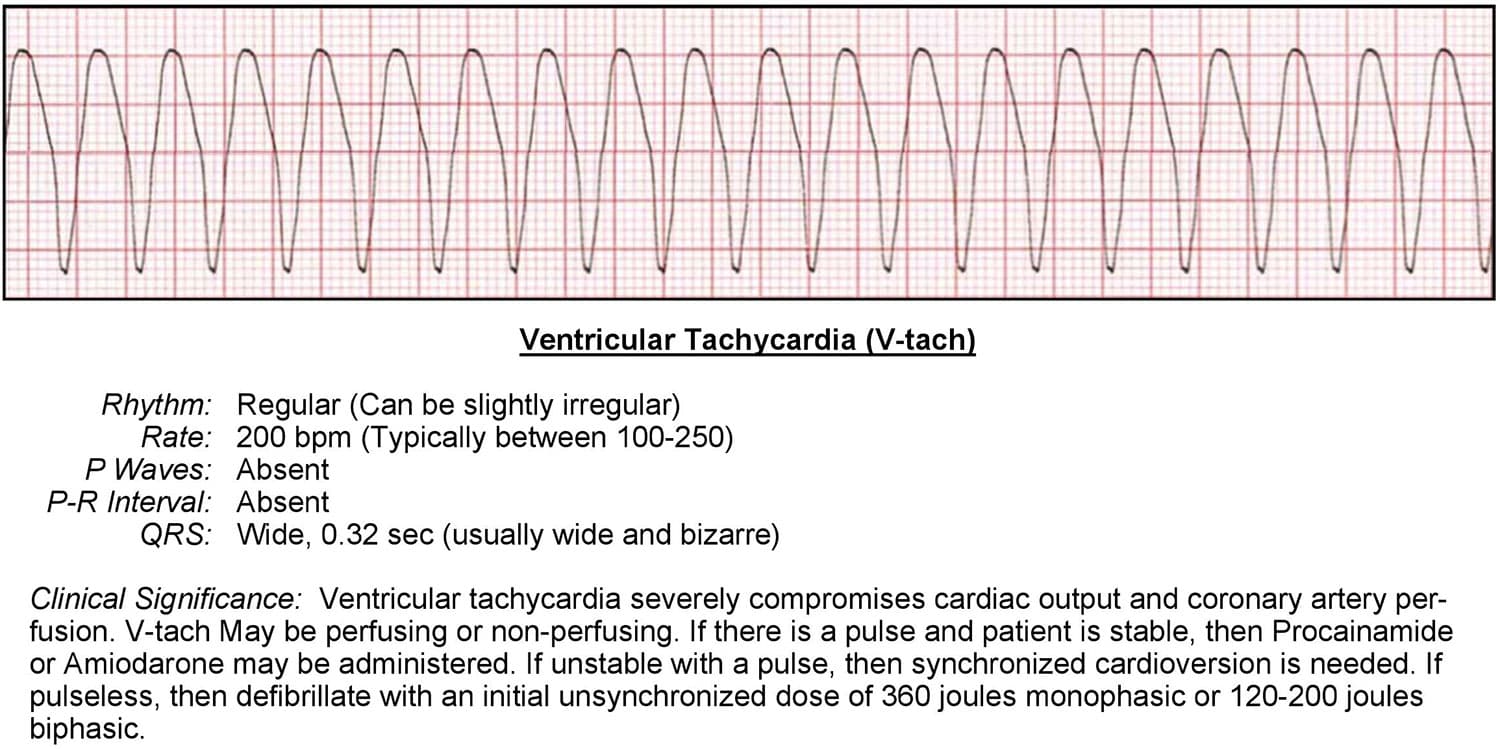
A very common ventricular tachycardia is monomorphic ventricular tachycardia. This means that all of the complexes are the same size, direction, and shape. This is usually caused by an ectopic pacemaker located in the ventricle.
An ECG will show the following:
- Rhythm is regular but may also be slightly irregular
- Rate is around 1 to 200 bpm
- Rarely any discernable P waves
- No discernable PR interval
- QRS complex is greater than .11 seconds and characterized as wide and bizarre
- No P wave to QRS ratio
The main problem with this type of fast wide complex tachycardia is hemodynamic instability. The heart rate is so fast that it inhibits the atrium from pre-filling and pre-loading the ventricles prior to their next contraction.
In this case, it is important for an ACLS team to know if the patient is stable or unstable. If stable, they will need to learn more about why the patient may be experiencing this arrhythmia.
Wide complex ventricular tachycardia can sometimes be caused by:
- Heart disease
- Electrolyte imbalance, especially in potassium
- QT interval prolongation
If the patient is stable, a 12-lead ECG should be ordered to see if the rhythm is supraventricular or ventricular in origin.
If the patient is unstable, immediate treatment is vital.
Wide Complex Polymorphic Ventricular Tachycardia
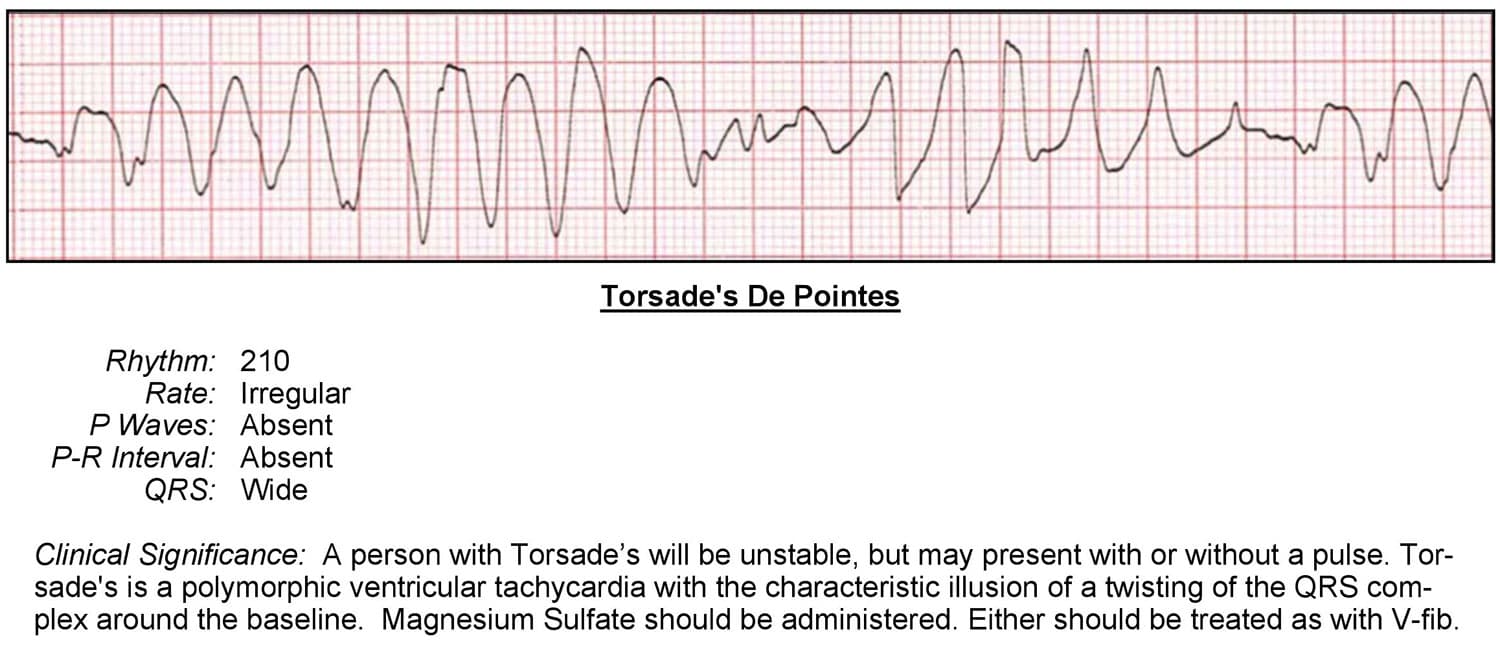
Poly, meaning multiple, describes the origin of the electrical foci in the ventricles. Polymorphic tachycardia is caused by multiple ventricular foci with the resulting QRS complexes varying in axis, amplitude, and duration.
It can also be described as bidirectional ventricular tachycardia—another type of polymorphic ventricular tachycardia.
Polymorphic ventricular tachycardia, known commonly as Torsades de pointes, is commonly associated with:
- Digoxin toxicity (most common association)
- Hypomagnesemia (low magnesium)
- Hypokalemia (low potassium)
Interpreting the ECG for polymorphic wide complex tachycardia:
- Rhythm is irregular
- Rate between 200-250 bpm
- No discernable P waves
- No PR interval
- QRS complex is variable but greater than .11 seconds and is wide and bizarre
- No P wave to QRS ratio.
In Torsades de pointes, it can sometimes appear that the QRS waves twist around from top to bottom and back again. Torsade de pointes (or TDP) translates as “twisting of points.”
The most important thing for professionals to remember with both monomorphic and polymorphic wide complex ventricular tachycardia is that both can become pulseless ventricular tachycardia or ventricular fibrillation very quickly.
Pulseless Ventricular Tachycardia
Wide complex ventricular tachycardia can present itself with or without a pulse. We can even see pulseless ventricular tachycardia in cardiac arrest patients, but in most cases, pulseless ventricular tachycardia quickly deteriorates into ventricular fibrillation.
Pulseless ventricular tachycardia is treated the same as ventricular fibrillation. It needs to be recognized and treated immediately.
The ECG interpretation can be the same as pulsed ventricular tachycardia, but the difference is that the patient is:
- Unresponsive
- Not breathing normally
- Pulseless